Children’s Eye Care

Children’s Eye Care
Children’s eyes are special, and they deserve someone who specializes in pediatric eye care. Sanjeev Dewan, M.D. of Ohio Eye Alliance is nearby to help.

Dr. Dewan specializes in eye problems children encounter. He can examine children at any age, even those who are too young to fully participate in their exam. Early detection of vision problems greatly is important as it improves the chances of successful treatment in children.

What is Strabismus?
Strabismus simply means eye misalignment, where the two eyes are looking at different images. In children with strabismus, one eye looks at one object of interest while the other eye points in, out, up or down.

Strabismus
How common is strabismus?
It is estimated that 4% of the U.S. population has strabismus.

*Click the links below to find out more Information.
-
Are there different types of strabismus and if so, how are they named?
There are many different types of strabismus. Strabismus is most commonly described by the direction of the eye misalignment. Common types of strabismus are esotropia (inturning), exotropia (outward turning), and hypertropia (a vertical misalignment of the eyes).
Strabismus can also be described by its cause. Three of the twelve cranial nerves (III, IV, VI) which arise from the brain and reaching the face are responsible for eye movement can be weak or palsied and cause strabismus. Some examples of this type of strabismus include third nerve (III) palsy, sixth nerve (abducens) and superior oblique (IV) palsy.
Special patterns of strabismus can have unique names such as Brown syndrome and Duane’s syndrome.
-
What are the types of horizontal strabismus?
Esotropia is inward turning of the eyes (aka “crossed eyes”). Types of esotropia include infantile esotropia, accommodative esotropia (related to farsightedness) and sixth nerve palsy. Exotropia is the term used to describe outward turning of the eyes (aka “wall-eyed”) [See figures 1 and 2].

Fig. 1: Large-angle infantile-onset esotropia.

Fig. 2: Child with exotropia of the right eye.
Regular and complete eye exams are of the utmost importance
for protecting your vision.To schedule your exam or learn more about your treatment options at Ohio Eye Alliance,
please call us today at (800) 423-6811. -
What are the types of vertical strabismus?
The terms hypertropia and hypotropia are used to describe vertical misalignment. Hypertropia is an abnormal eye higher than the normal eye. Hypotropia is when the abnormal eye is lower than the normal eye. The terms can generally be interchanged depending upon which eye is being described.
-
What causes strabismus?
Most strabismus is the result of an abnormality of the neuromuscular (including brain) control of eye movement. Our understanding of these control centers in the brain remains incomplete. Less commonly, a problem with the actual eye muscle may cause strabismus.
-
How is strabismus related to poor vision?
Eye misalignment is a major cause of amblyopia in children. When the eyes are oriented in different directions, the brain receives 2 different visual images. The brain may ignore the image from the misaligned eye to avoid double vision, resulting in poor vision development of that eye. Also, an eye that sees poorly may become misaligned.
-
Who develops strabismus as a child?
Strabismus often occurs in children who are otherwise completely normal. However, disorders that affect the brain such as Cerebral Palsy, Down syndrome, hydrocephalus and brain tumor are more likely to develop strabismus.
-
What adult disorders cause strabismus?
Stroke or vascular problems may cause strabismus in adults. Trauma, neurological problems, and Grave’s disease (thyroid eye disorders) are other common causes of strabismus.
-
How does trauma cause strabismus?
Trauma can cause strabismus by:
Brain Damage that impairs control of eye movement,
• Damage of the nerves that control eye movement and/or
• Damage of the eye muscles either directly or secondarily from trauma to the eye socket. -
How is strabismus treated?
The goal of strabismus treatment is to improve eye alignment which allows for the eyes to better work together (binocular vision). Treatment may involve eye glasses, eye exercises, prism, and/ or eye muscle surgery. The underlying problems associated with strabismus (including ptosis and cataract) are usually treated prior to eye muscle surgery, and amblyopia may be treated before or after surgery.
Amblyopia
Children with strabismus frequently have an associated condition called amblyopia (lazy eye), although amblyopia can occur without any eye misalignment. Here, one or both eyes have reduced visual acuity.

What is Amblyopia?
Amblyopia is decreased vision in one or both eyes due to abnormal development of vision in infancy or childhood. In amblyopia, there may not be an obvious problem of the eye. Vision loss occurs because nerve pathways between the brain and the eye aren’t properly stimulated. The brain “learns” to see only blurry images with the amblyopic eye even when glasses are used. As a result, the brain favors one eye, usually due to poorer vision in the other eye. Another word for amblyopia is often “lazy eye.” It is the leading cause of vision loss amongst children. [See figure 1]

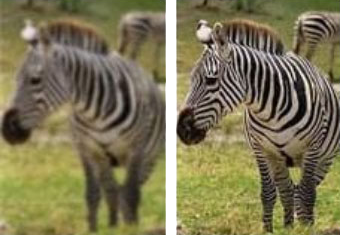
Fig. 1: Blurred view (left) and Normal view (right)
-
What causes amblyopia?
Normal vision develops during the first few years of life. At birth infants, have very poor vision, however as they use their eyes the vision improves because the vision centers in the brain are developing. If infants are not able to use their eyes from various reasons the vision centers do not develop properly and the vision is decreased despite normal appearance of the structures of the eyes.
The most common cause is refractive error in one or both eyes that is not corrected early in childhood resulting in poor development of the visual function in the affected eye/s. This is called refractive amblyopia. Another common cause is strabismus or eye misalignment. This is called strabismic amblyopia.
Rarely there is a structural anomaly that impairs the visual function like a droopy eyelid or opacity in the visual axis like cataract or corneal scar. This is called deprivation amblyopia.
Multiple causative factors can coexist.
-
What is strabismic amblyopia?
Strabismic amblyopia develops when the eyes are not straight. One eye may turn in, out, up or down. When this happens, the brain begins to ignore, or “turns off” connection to the eye that is not straight and the vision subsequently drops in that eye. -
What is deprivation amblyopia?
Deprivation amblyopia develops when cataracts or similar conditions “deprive” young children’s eyes of visual experience. If not treated very early, these children never learn to see very well and can have very poor vision. Sometimes this kind of amblyopia can affect both eyes. -
What is refractive amblyopia?
Refractive amblyopia happens when there is a large or unequal amount of refractive error (glasses strength) between a child’s eyes. The brain learns how to see well from the eye that has less need for glasses and does NOT learn to see well from the eye that has a greater need for glasses. The vision problem may be invisible because the child does not complain of blurry vision. The child sees well with the better seeing eye. Additionally, the amblyopic eye may not look any different from the normal seeing eye. Therefore, parents and pediatricians may not think there is a problem because the child’s eyes look normal. For these reasons, this kind of amblyopia in children may not be found until the child has a vision test. This kind of amblyopia can affect one or both eyes and can be best helped if the problem is found early. -
Will glasses help a child with amblyopia to see better?
Glasses may improve visual acuity to some degree but usually not completely. With amblyopia, the brain is “used to” seeing a blurry image and needs to learn how to see better with that eye. With time, however, the brain may “re-learn” how to see and the vision may increase. The normal eye is treated (most often with patching or eyedrops) to make the amblyopic (weak) eye stronger. -
What can be done if my child has equal high amounts of farsightedness and/or astigmatism and is diagnosed with bilateral amblyopia?
Bilateral amblyopia is usually treated with consistent, early glasses, and or contact lenses with follow-up over a long period of time. If asymmetric amblyopia (one eye better than the other) occurs, then patching or eye drops may be added. -
When should amblyopia be treated?
Early treatment is always best. If necessary, children with refractive errors (nearsightedness, farsightedness or astigmatism) can wear glasses or contact lenses when they are as young as one week old. Children with cataracts or other “amblyogenic” conditions are usually treated promptly in order to minimize the development of amblyopia. -
How old is too old for amblyopia treatment?
Early treatment is always best. If necessary, children with refractive errors (nearsightedness, farsightedness or astigmatism) can wear glasses or contact lenses when they are as young as one week old. Children with cataracts or other “amblyogenic” conditions are usually treated promptly in order to minimize the development of amblyopia. -
How can I get early treatment for amblyopia?
Some forms of amblyopia, such as that associated with large-deviation strabismus, may be easily detected by parents. Other types of amblyopia (from high refractive error) might cause a child to move very close to objects or squint his or her eyes. Still other forms of amblyopia may NOT be obvious to parents and therefore must be detected by Vision Screening. -
What is vision screening?
Vision Screening is strongly recommended by the American Academy of Pediatrics (AAP) over the course of childhood to detect amblyopia early enough to allow successful treatment. Pediatricians check newborns for red reflex to find congenital cataracts. Infants are checked for the ability to fix and follow and whether they have strabismus. Toddlers can have their pupillary red reflexes tested with a direct ophthalmoscope (Brückner Test) or by instruments that identify a significant refractive error that needs correction to prevent amblyopia. When children can consistently identify objects either by reading or by matching, the acuity of each eye (with the non-tested eye patched) is screened to identify amblyopia. -
How is amblyopia treated?
One of the most important treatments of amblyopia is correcting the refractive error with consistent use of glasses and/or contact lenses. Other mainstays of amblyopia treatment are to enable as clear an image as possible (for example, by removing a cataract), and forcing the child to use the weaker eye (via patching or eye drops to blur the better-seeing eye). -
When should patching be used for amblyopia treatment?
Patching is a very effective way of treating amblyopia as it allows the weaker eye to get stronger, however it is very hard to make a young child wear a patch. It needs a lot of effort, persistence and encouragement from the parents. The younger the child is, the faster it works in improving the vision, therefore the parents should be persistent and encouraging and not wait until the child is old enough to want to patch. An ophthalmologist should regularly check how the patch is affecting the child’s vision. -
Are there different types of patches?
The classic patch is an adhesive “Band-Aid” which is applied directly to the skin around the eye. They are available in different sizes for younger and older children. For children wearing glasses, both cloth and semi-transparent stickers (Bangerter foils) may be placed over or onto the spectacles. “Pirate” patches on elastic bands are especially prone to “peeking” and are therefore only occasionally appropriate. Good quality felt patches which wrap completely around one lens of eyeglasses are available on various sites. -
Is there an alternative to patching to treat amblyopia?
Sometimes the stronger (good) eye can be “penalized” or blurred to help the weaker eye get stronger. Atropine drops will temporally blur the vision in the good eye, especially for near activity and work as a great alternative to patching in selected cases. This forces the child to use the weaker eye. For mild to moderate degrees of amblyopia, studies have shown that patching or eye drops may be similarly effective. Dr. Dewan often uses a combination of patching and Atropine drops to treat amblyopia, as their effects are complementary. -
Do drops work for all amblyopic children?
Not all children benefit from eye drop treatment for amblyopia. Penalizing eye drops (such as atropine) do not work as well when the stronger eye is nearsighted or when the degree of amblyopia is severe. -
How many hours per day patching is enough when treating amblyopia?
The mainstay of treating amblyopia is patching of the dominant (good) eye, either full or part-time during waking hours. The prescribed number of hours of patching will depend on the visual acuity in the amblyopic eye and whether treatment has been successful in the past. Your doctor will prescribe the appropriate time for you. -
How long does amblyopia patching therapy take to work?
Although vision improvement frequently occurs within weeks of beginning patching treatment, optimal results often take many months. Once vision has been improved, less (maintenance) patching or periodic use of atropine eyedrops may be required to keep the vision from slipping or deteriorating. This maintenance treatment may be advisable for several months to years. -
During which activities should patching be performed?
Any activity that requires the active visual attention of the child will encourage more effective return of vision during amblyopia treatment. Near activity in particular (such as reading, coloring hand held computer games) during treatment may be more stimulating to the brain and produce better or more rapid recovery of vision. The most important part of treatment is keeping the patch on for the prescribed treatment time. As long as the child is conscious and has his or her eyes open, visual input will be processed by the amblyopic eye. On the other hand, the child may be more cooperative or more open to bargaining if patching is performed during certain, favorite activities (such as watching a preferred television program or video). -
Should patching be performed during school hours?
In many instances, school is an excellent time to patch, taking advantage of a period of active visual attention. While in most instances, children may not need to modify their school activities while patching, sometimes adjustments such as sitting in the front row of the classroom will be necessary. If the patient, teacher, and classmates are educated appropriately, school patching need not be a socially stigmatizing experience. On the other hand, frequently a parental or other family figure may be more vigilant in monitoring patching than is possible in the school setting. Parents should be flexible in choosing when to schedule patching. -
What if my child refuses to wear the patch?
Many children will resist wearing a patch at first. Successful patching may require persistence and plenty of encouragement from family members, neighbors, teachers, etc. Children will often throw a temper-tantrum, but then they eventually learn not to remove the patch. Another way to help is to provide a reward to the child for keeping the patch on for the prescribed time period. A combination of persuasion, reward and most of all, love will be most effective. -
What happens if amblyopia is not treated?
If amblyopia is not treated the vision in the affected eye/s will be permanently decreased causing deficits in depth perception and peripheral vision. Moreover if the good eye becomes injured or affected by a disease, significant lifetime disability may result. The ophthalmologist will give the instructions and monitor the progress but the patient and the family will do the hard work of actually performing the treatment. Children do not like to have their good eye patched, especially if the vision in the amblyopic eye is very low, but parents must stand by them and help them do what’s best. Parents play probably the most important role in a successful treatment. -
Can surgery be performed to treat amblyopia?
There is no surgery to improve the vision for amblyopia. Surgery can be performed to straighten misaligned eyes such as crossing. Surgery to make the eyes straight can only help enable the eyes to work together as a team. Children with strabismic amblyopia still need close monitoring and treatment for the amblyopia, and this treatment is done either before or after strabismus surgery is performed.
Children who are born with cataracts may need surgery to take out the cataracts. After surgery, the child will usually need vision correction with glasses or contact lenses and patching.
-
What are appropriate goals of amblyopia treatment?
In all cases, the goal is the best possible vision in each eye. While not every child can be improved to 20/20, most can obtain a substantial improvement in vision. The earlier the treatment for amblyopia, the more successful the treatment tends to be. -
What happens if amblyopia treatment does not work?
If amblyopia is not treated the vision in the affected eye/s will be permanently decreased causing deficits in depth perception and peripheral vision. Moreover, if the good eye becomes injured or affected by a disease, significant lifetime disability may result.

From the American Association for Pediatric Ophthalmology and Adult Strabismus, AAPOS.org.

